A recent study published in the New England Journal of Medicine has alarmingly revealed that new tuberculosis (TB) strains, resistant to the latest treatment regimens, are being transmitted between patients globally. This groundbreaking research, led by the Swiss Tropical and Public Health Institute (Swiss TPH), contributes to the growing concern over antimicrobial resistance and its profound implications for global health.
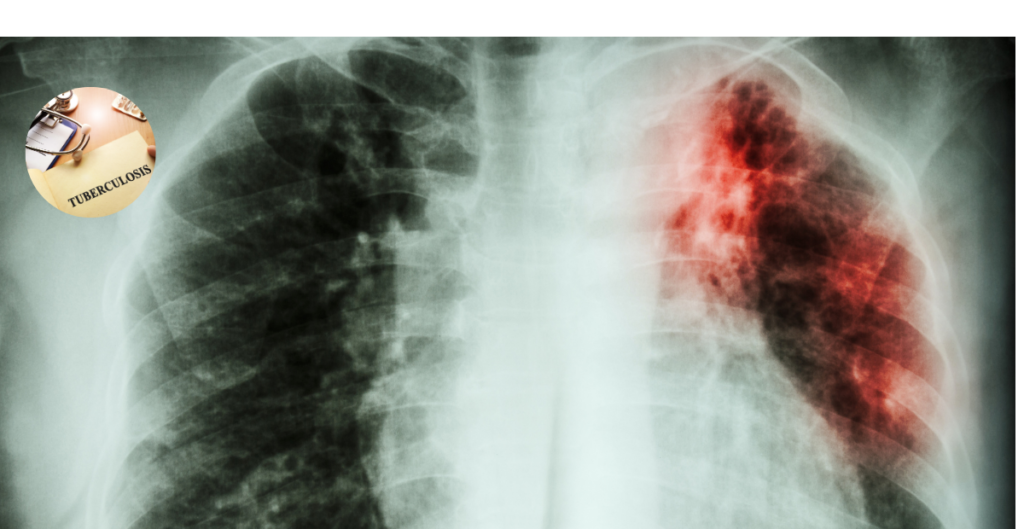
TB remains the world’s leading infectious disease killer, claiming approximately 1.25 million lives annually. The emergence of multidrug-resistant TB (MDR-TB) has significantly complicated the global response to this pandemic. In 2022, the World Health Organization (WHO) endorsed a novel 6-month treatment regimen, BPaL(M), following evidence of its improved safety and efficacy. However, the latest study indicates that TB bacteria are rapidly adapting to this new regimen, highlighting the urgent need for enhanced surveillance and infection control measures.
By analyzing the genomes of nearly 90,000 M. tuberculosis strains from around the world, the Swiss TPH researchers identified 514 strains resistant to TB drugs, including both old and new treatment regimens. Alarmingly, 28% of these highly drug-resistant strains were transmitted directly from one patient to another, with cases found in 27 countries across four continents.
The authors observed that the new treatment regimen marks a substantial improvement for patients suffering from multidrug-resistant tuberculosis (MDR-TB). However, they anticipated that overcoming Mycobacterium tuberculosis would prove to be a considerable challenge. Therefore, it was crucial to explore how the bacteria would react to the global adoption of this innovative treatment protocol.
Furthermore, experts underscore the importance of integrating these novel medications with comprehensive diagnostics and surveillance systems to mitigate the risk of developing drug resistance. Enhanced diagnostic tools, effective infection control measures, and strong surveillance frameworks are crucial for limiting the proliferation of these highly drug-resistant strains and preserving the effectiveness of the new treatment protocols.
As the world searches for ways to improve diagnosis of Tuberculosis, Artificial Intelligence is offering a new frontier. However, there is need for human oversight in the development and deployment of Artificial Intelligence (AI) in healthcare. For instance, AI-powered diagnostics and decision-making tools, especially for diseases like tuberculosis, can lead to misdiagnosed cases or missed crucial signs, resulting in improper treatment recommendations. Therefore, a balanced approach, combining AI’s potential with careful design, regulation, and human oversight, is crucial for ensuring fair and accurate decision-making in complex environments.
Addressing Antimicrobial Resistance
The swift rise of drug-resistant tuberculosis (TB) strains underscores a significant challenge facing the global health community: antimicrobial resistance. Addressing this issue necessitates proactive measures in the ongoing battle between drug development and the evolution of bacterial resistance. The authors acknowledge that, on a positive note, the overall number of these cases remains relatively low. However, it is concerning that over a quarter of these highly drug-resistant cases result from patient-to-patient transmission, just two years after the World Health Organization (WHO) endorsed a new treatment regimen.
Conclusion
The study’s findings have far-reaching implications for public health policy and interventions. As the world grapples with the growing threat of antimicrobial resistance, the urgent need for standardized diagnostic tools, enhanced infection control measures, and robust surveillance systems cannot be overstated. By acknowledging the limitations of AI in high-stakes environments and embracing a mixed approach that combines technological advancements with human insight, we can better safeguard the efficacy of novel treatment regimens and ultimately, save lives.
Galo A. Goig et al, Transmission as a Key Driver of Resistance to the New Tuberculosis Drugs, New England Journal of Medicine (2025). DOI: 10.1056/NEJMc2404644